Alternatively titled: Yellow Fever. Penny-wise, Pound Foolish. Sir Andrew Witty’s Model Minorities
Chinese (and, generally, Asian) Americans are one of the most attractive consumer segments in the insurance business. As illustrated below, they tend to be lower utilizers, ~58% lower than white Americans. This makes them attractive to payers trying to minimize their medical expenditures and a number of risk-bearing groups have built their model on this premise: rendr, Clever Care, Astrana and their recent co-branded MA Plan with SCAN.
It made me wonder what a health plan tailored to the unique healthcare needs of the Chinese American community might look like, beyond the platitudes of culturally sensitive care (platitudes can be true!). Less on the how and more on the what: what conditions were Chinese people uniquely at risk for? What kinds of (medical expense-driving) clinical interventions would one need to address them?
What are Chinese health problems?
Some quick hits: lactose intolerance, hepatitis B, mental health…data issues with devastating consequences sharply articulated here…all very important but for the sake of applying a population health lens I’m focusing on:
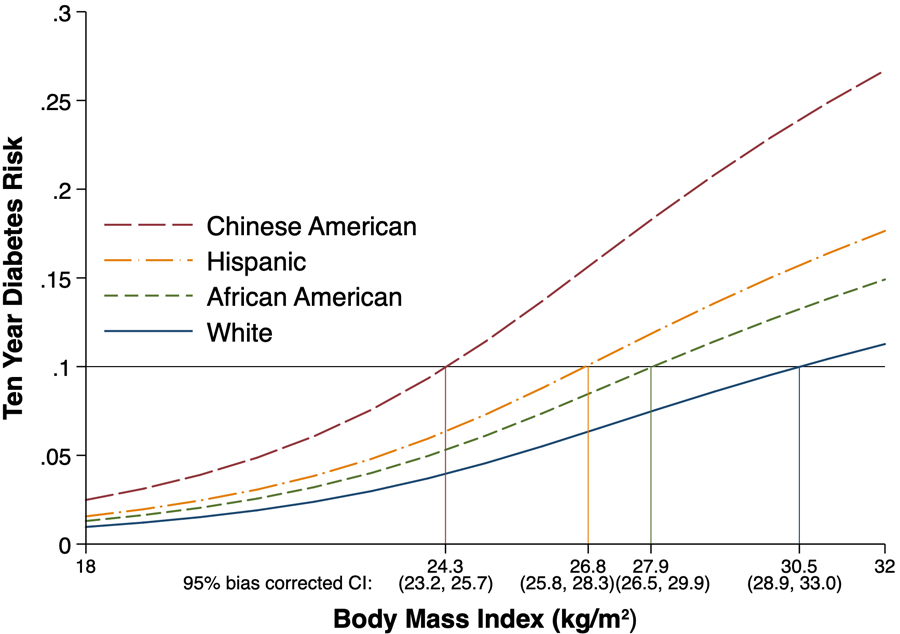
Increased Diabetes risk at Lower BMIs
A study based on the longitudinal Multi-Ethnic Study of Atherosclerosis (MESA) found that obese, adult Chinese Americans have 2.5x the diabetes risk of white Americans in the same weight range (BMI >30). Lest you attribute this Chinese Americans being generally healthier, they also found that Chinese Americans reach the same diabetes risk as an obese white American at a BMI of 24.3 – within the healthy weight limit.
These findings were consistent with other research which has found that South Asians and Latinos reach the diabetes risk level of white peers at much lower BMIs.
Diagnosed diabetes in the United States is higher among people of color to begin with, and these studies support research that shows Asian Americans are twice as likely to be undiagnosed (8% vs. 4% for white Americans).
In a world where doctors (and patients) only start to screen for diabetes when a patient is obese, diabetic, normal weight Chinese Americans are more likely to slip under the radar.
Cardio-metabolic disease?
Weight is but one of the adverse health outcomes we should be concerned about and as we’ve seen with diabetes it is an inadequate leading indicator for Chinese Americans’ unique physiology. High blood pressure and high cholesterol (dyslipidemia) are also part of the cluster of symptoms known as cardio metabolic disease that create a negative feedback loop of insulin resistance and deteriorating metabolism, ultimately driving early death in the western world. As Peter Attia describes in Outlive, it’s this – not necessarily visible fat itself – that we care about, and researchers estimate that as much as a third of the afflicted population is not obese. Like with diabetes, BMI is just a leading indicator for dangerous fat accumulation and increasing lipid load. For better studied physiologies, fat builds up subcutaneously before the deposits are filled and it begins gathering in your organs (visceral). That’s when non-fatty alcholic liver disease progresses and your metabolism may start to go haywire. It someone had small subcutaneous fat deposits but ate unhealthily, they’d actually start facing the negative health outcomes sooner! It’s not hard to imagine that Chinese Americans are a disproportionate share of this “skinny fat” cohort.
What should the care model look like?
Interestingly, not only are these relatively cheaply diagnosed, but the insurance-favored intervention could be culturally aligned! My Chinese American mother illustrates this well: after being flagged for pre-diabetes and heart abnormalities by her PCP, she bought herself a cheap holter monitor online. She thought the glucose test was invasive and wanted to check it sparingly and, although the doctor offered statins, she wanted to delay any prescriptions as along as possible. She started monitoring her processed food intake and walking every day. She might have started taking a daily herbal tea. When her monitored heart rate stabilized, she followed up with her doctor to be tested again and her A1c was controlled. She never took traditional medication or saw an additional specialist. An insurance company’s dream!
Plugging some silly little numbers affirms the financial appeal
Illustrative Pro Forma for a Chinese American-Focused Plan on the NYS Exchange (PMPY)
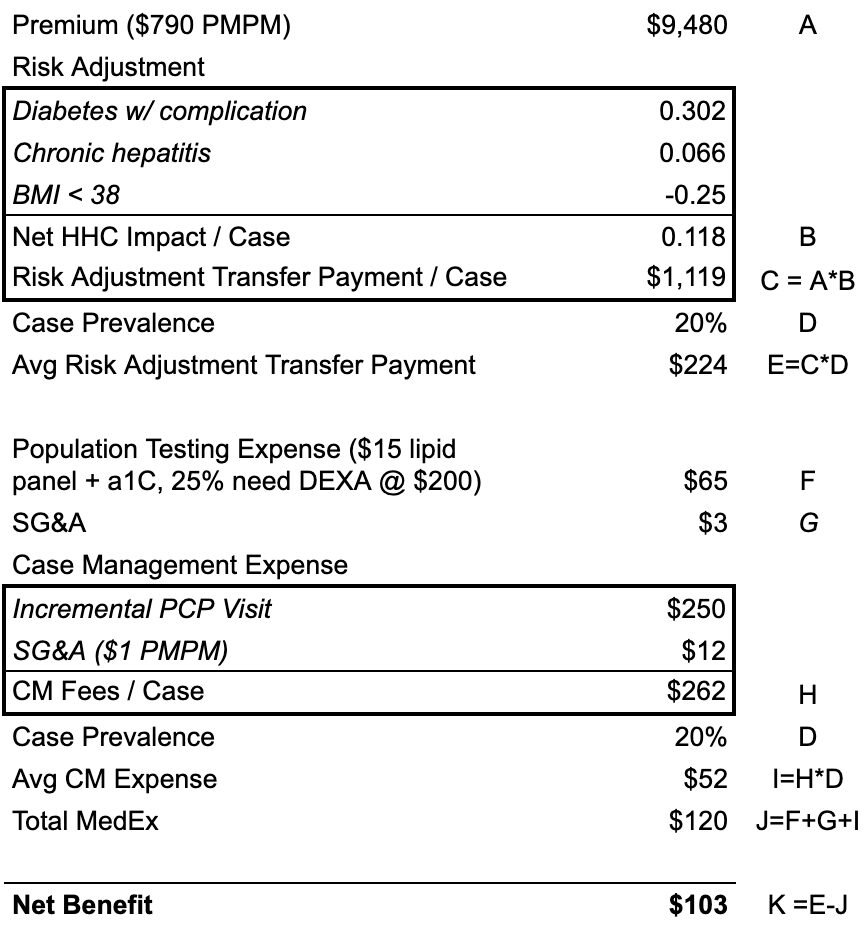
Source: author 🧠 🤔
I’m no actuary and these aren’t crazy Medicare Advantage margins, but it goes to show one could design a plan providing ethnically appropriate, reasonably rich screening benefits to the population, pay PCPs fairly, and still come out ahead through the savings on treatment. Sprinkle on a lactaid benefit and maybe you can attract a large enough healthy population to subsidize some DMEs!
I’d love to see how the lifestyle intervention-based disease management programs beloved by payers resonate with Chinese people or might be otherwise “localized” (is your grandma calling you 肥嘟嘟 to shame you out of dessert not her take on glucose restricted diet coaching?). I wonder if it would accelerate clinical research in Traditional Chinese Medicine.
All that said, this is a thought experiment. I hope any readers of color take their metabolic health seriously – before their BMI skyrockets – but it shouldn’t discredit mainstream public health guidelines. Just like heart disease, not breast cancer, is the number one cause of premature death in women, identitarian concerns shouldn’t prevent us from addressing the health risks that afflict all us leading the modern western lifestyle.
What do you think? What health problems are important to your community? Are you seeing them meaningfully addressed in the healthcare space? I want to know!

Leave a Reply